
Click the triangle below to listen to the podcast brief and access the transcript by clicking here.
Introduction
As skin heals from a burn injury, it may get itchy. Almost everyone recovering from major burns has problems with itching—especially on or around the burn, graft, or donor site. The medical term for itchiness is “pruritus” (proo-ri´tus).
Itching is a normal part of healing. The reasons it happens are likely complex and poorly understood. Itch intensity (how bad it is) and frequency (how often it occurs) are not necessarily related to the size or depth of your burn injury, but itching may cause you to scratch and open up fragile skin that previously had healed.
Itching can also get in the way of doing everyday activities, including:
- Sleep: Itching tends to worsen at night, making it hard to fall asleep and stay asleep.
- Work and school: Persistent itching may make it hard to concentrate when performing these activities.
- Physical activities: Exercise, sports, and play (for children) may increase itching.
Itching can make you anxious, which can make itching worse. Fortunately, itching decreases over time. In the meantime, there are treatments to help reduce itching. To find the best treatment for you, talk with your health care team about how bad your itching is and how it is affecting your life.
Ways to Describe Your Itching
Your health care team may ask you to describe the intensity and impact of your itch:
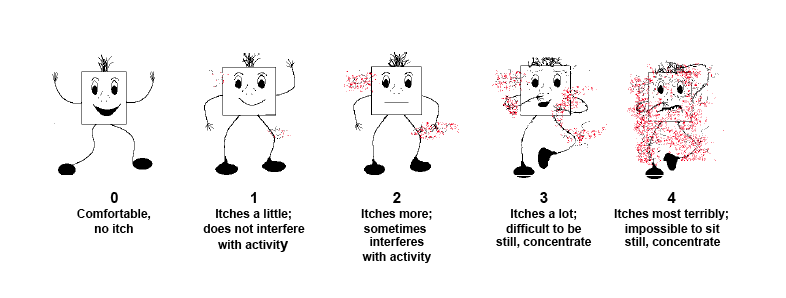
- To describe intensity, or how strong the itch is, adults are usually asked to rate the itching on a scale of 0 to 10, where 0 is “no itch” and 10 is “worst itch imaginable.” Children are often asked to use the Burn Man Itch Scale to describe their itch (see below).
- To describe how itching may be affecting your life, your health care team may use the 5-D Itch Scale. This is a set of questions that asks you about the
- Duration (number of hours per day)
- Degree (intensity)
- Direction (whether it is getting better or worse)
- Disability (impact on activities)
- Distribution (location on your body)
You can also use the questions in the 5-D Itch Scale to initiate conversations with your health care providers.
Treatment
No treatment stops itching completely, but several may help.
Topical Therapies
Creams and lotions
- Moisturizers help to maintain skin moisture and hydration. They may help reduce itching if your skin is dry, because itching increases with dry skin. Use unscented or fragrance-free moisturizers. Applying moisturizers more frequently may be helpful.
- Diphenhydramine (pronounced dai-fen-hai-dremine; abbreviated DPH or DHM) cream blocks histamine and is sometimes helpful. Histamine is a naturally occuring compound in our bodies that triggers the inflammatory response. It is available over the counter and does not require a prescription.
- Doxepin cream (e.g., Zonalon or Prudoxin) has been used with some success. It decreases itching by blocking histamine receptors in the skin. Doxepin creams can be used only in small amounts and must be prescribed.
- Capsaicin (pronounced cap-SAY-sin) cream (e.g., Capzasin, 0.025%) may provide temporary relief. It is best to test this cream on a small area of your skin first because it may cause a stinging or burning sensation, particularly with the first few applications. Avoid getting capsaicin cream in your eyes and other mucous membranes or on broken skin. Wash your hands with soap and water after applying (unless your hands are within the treatment area). If applying to your hands, wait 30 minutes before washing your hands.
Baths
- Bathing may or may not help with itching. Lukewarm water is best and tends to dry out skin the least.
- Bath additives such as oatmeal, powdered milk, or baby oil can be helpful.
- Cooling the skin with water provides some temporary relief.
Oral Medications
- Antihistamines work by blocking histamine, which triggers itching. Common antihistamines used include diphenhydramine (e.g., Benadryl), cetirizine, loratadine, and hydroxyzine. They can be purchased over the counter, either as pills for adults or elixirs or liquids for children. Dosages (how much you should take) vary, so talk with your health care provider before taking any over-the-counter medications.
- Gabapentin (pronounced gab-ah-pen-tin) is an oral medication that must be prescribed. It acts centrally—in your brain—to help decrease itching and has shown promising results in several research studies.
- Sleep medications are used to treat sleeplessness (insomnia). Medications can sometimes be helpful to get to sleep and stay asleep. If itching makes it difficult for you to sleep, talk with your health care provider about safe sleep medications that can help.
- Before taking any medication, talk to your doctor about the side effects.
- Other medications may be helpful in decreasing postburn itching - talk with your healthcare provider about your options. Ask your doctor or health care provider to review all your medications as some medicines can cause itching.
Other Tips
- Custom-fit pressure garments and other supportive dressings (e.g, Tubigrip Elastic Tubular Bandage) or tight fitting sport clothing may help during the first months to year following burn injury.
- Skin massage with lotion and/or touching with firm pressure on healed areas can help reduce itching. Make sure you check with your healthcare provider if your itching remains bothersome. In some cases, other treatments such as steroid injections, laser treatments or even surgery can be helpful.
- Distractions such as television, games, and low-impact or mild exercise or activities can help take your mind off the itching.
- Short fingernails, especially for children who tend to scratch at night while asleep, can reduce injury to fragile skin.
- Use unscented laundry detergent.
- Use unscented or fragrance-free lotions (including sunscreens).
- Protect your skin from the sun by wearing appropriate clothing (e.g., a hat and long sleeves) and using sunscreen.
For More Information
- The Phoenix Society for Burn Survivors: http://www.phoenix-society.org/
- American Burn Association: http://www.ameriburn.org/
- In addition, you can contact your health care providers about local support groups and other resources.
References
Carrougher GJ, Martinez EM, McMullen KS et al. Pruritus in adult burn survivors: post-burn prevalence and risk factors associated with increased intensity. J Burn Care Res. 2013;34(1):94-101.
Elman S, Hynan LS, Gabriel V, Mayo MJ. The 5-D itch scale: a new measure of pruritus. Br J Dermatol. 2010;162(3):587-93.
Morris V, Murphy LM, Rosenberg M, Rosenberg L, Holzer CE 3rd, Meyer WJ 3rd. Itch assessment scale for the pediatric burn survivor. J Burn Care Res. 2012; 33(3):419-24.
Schneider JC, Nadler DL, Herndon DN, Kowalske K, Matthews K, Wiechman SA, Carrougher GJ, Gibran NS, Meyer WJ, Sheridan RL, Ryan CM. Pruritus in pediatric burn survivors: defining the clinical course. J Burn Care Res. 2015 Jan-Feb; 36(1)151-8.
Authorship
Itchy Skin After Burn Injury was developed by Gretchen J. Carrougher, R.N., M.N., and Walter J. Meyer III, M.D., in collaboration with the Model Systems Knowledge Translation Center.
Factsheet Update
This factsheet was reviewed and updated by Gretchen Carrougher MN, RN, Northwest Regional Burn Model System; Karen Kowalske, MD, University of Texas Southwestern; Jeffrey C. Schneider, MD, Colleen M. Ryan, MD, and Barbara A. Gilchrest, MD, Boston-Harvard Burn Injury Model System. The review and update is supported by the American Institutes for Research Model Systems Knowledge Translation Center.
Source: Our health information content is based on research evidence whenever available and represents the consensus of expert opinion of the Burn Injury Model System directors.
Disclaimer: This information is not meant to replace the advice from a medical professional. You should consult your health care provider regarding specific medical concerns or treatment. This publication was produced by the Burn Model Systems in collaboration with the University of Washington Model Systems Knowledge Translation Center with funding from the National Institute on Disability and Rehabilitation Research in the U.S. Department of Education, grant no. H133A060070. It was updated under the American Institutes for Research Model Systems Knowledge Translation Center, with funding from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90DP0012). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS).
Copyright © 2016 Model Systems Knowledge Translation Center (MSKTC). May be reproduced and distributed freely with appropriate attribution.
Other Languages
The Itchy Skin After Burn Injury factsheet is also available in Amheric, Arabic, Russian, Somali, Tigrinya, and Vietnamese.