What Is Functional Electrical Stimulation?
People with a spinal cord injury (SCI) often have weakness in their arm, leg, or trunk muscles. This weakness may be partial or complete, making some movements difficult or impossible. In many cases, functional electrical stimulation (FES) can help with weak muscles. FES delivers small electrical pulses to weak muscles. This helps muscles to contract and move body parts in useful ways. FES uses sticky pads called electrodes to deliver the pulses in a controlled manner. The electrodes go directly on the skin over the target muscles.
FES can help produce a leg or arm cycling motion or a hand grasping motion. It can also help with standing, coughing, walking, and some arm or hand tasks. Its effect depends on how the electrical pulses activate the leg, hip, arm, shoulder, or trunk muscles.
When you use FES, you may notice contraction of your muscle, but not pain or an electrical shock. Tell your health care provider if you have pain when using FES or if your skin breaks down in the area of the electrodes.
How Is FES Used With SCI?
- You can use FES during physical or occupational therapy. It can help you to regain muscle strength. If used routinely while practicing movements, FES may help regain some control of movements.
- You can combine FES with braces, splints, or orthotics to help you stand and/or walk or grasp an object and/or move your wrist, elbow, shoulder.
- You can use FES as part of a regular exercise program with or without exercise equipment.
- You can use FES at home to help maintain healthy muscles and heart health.
What Types of FES Devices Are Available?
There are many FES devices that you could use in your rehabilitation program. Availability, features, and insurance coverage vary by treatment site. Talk with a health care provider who has experience with FES systems and SCI to figure out if FES may work for you and which FES device will meet your needs and goals.
Here are some common FES devices:
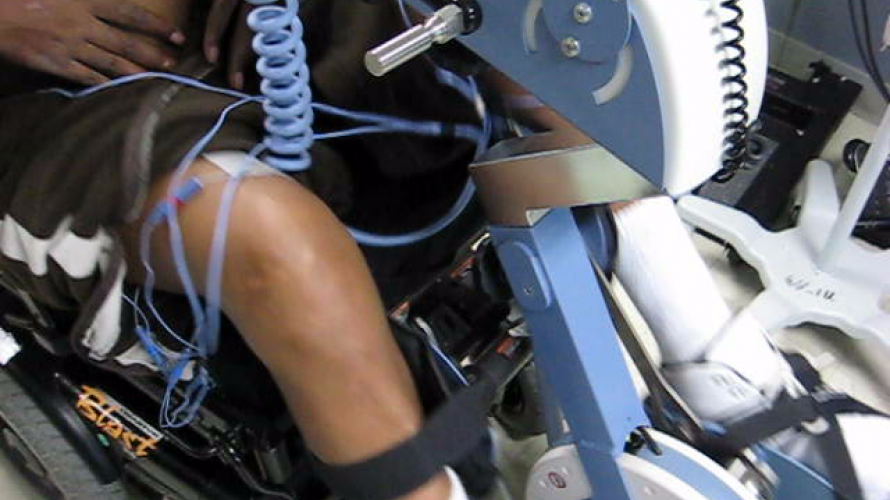
- FES cycling. You can use this device for leg or arm cycling exercises. It uses a stationary bike or a handcrank with built-in electrical stimulation. Electrodes go on the skin over arm or leg muscles. Electrical pulses produce muscle contractions. This device may help people with little or no leg or arm function to pedal their legs or crank their arms.
- FES upper limb. This device stimulates the muscles in the arm and hand. It uses electrodes that go on the skin over the shoulder, arm, or hand muscles. Electrical pulses activate the muscles that cause your arm or hand to produce a desired movement, such as grasping an object or lifting weights.
- FES rowing. This device stimulates the leg muscles while allowing users to voluntarily engage their upper extremity muscles simultaneously while in a seated position. As users pull with their arms, electrical pulses stimulate their front thigh muscles to extend their legs. Once in an extended position, the electrical pulses stimulate the back thigh muscles to return to the start position.
- FES lower limb and trunk. This device helps with weight shifting, balancing, standing, transferring, and walking. Electrodes go on the skin over the leg or trunk muscles. Electrical stimulation produces and coordinates hip, leg, and trunk movements.
- Portable and wearable FES devices. These are small, mobile FES devices that are worn on the body to produce movement. They use pads or sleeves to hold the electrodes in place over the targeted muscles. These devices work best for daily use.
- Implanted FES. Some FES devices are implanted inside the body with electrodes implanted on nerves or muscles to restore function or control. They provide constant electrical stimulation. People with long-term or chronic issues may benefit from these systems. As of 2023, these devices are exclusively used in research studies. To view a list of studies using implanted FES systems, search ClinicalTrials.gov or SCITrials.org.
Is FES Right for Me?
Talk to your doctor and therapist to find out if FES is right for you. Your doctor and therapist can work with you to develop an FES program that fits your goals. They will confirm that you are eligible to take part in an FES program. They will also make sure that it is safe for you.
Who May Benefit From FES?
FES may help many people who have lost some or all their muscle function due to an SCI. FES may not work if the SCI damaged the nerves outside of your spinal cord (called peripheral nerves) that connect to the muscles. You may experience discomfort if you have feeling where the electrodes go. Pain could limit how much you use FES devices.
When Should I Not Use FES?
- Do not use FES if you are pregnant or have any cancer other than skin cancer that has not spread.
- Your doctor will need to approve FES if you have certain types of pacemakers.
- Never place the electrodes over your eyes, on the front of your neck, or over any broken skin or wounds.
- Stop using FES if autonomic dysreflexia or a seizure occurs.
- Don’t use FES if you have had a blood clot or a fracture within the last 3 months.
- If you have a skin reaction or your skin breaks down in the area of the electrodes, stop using them. Ask your therapist or doctor if there are other electrodes that you can use.
What Are the Potential Benefits of FES?
FES works your muscles. As a result, it has benefits that are similar to exercise. Like an exercise program, getting into a routine and following your FES program can benefit your health.
Direct benefits of FES may include:
- Maintained or improved the size of stimulated muscles and muscles near the stimulated muscles.
- Maintained or improved the strength of your stimulated muscles.
- Improved ability to control movements that have been practiced.
- Improved blood circulation.
- Reduced spasticity in stimulated and nearby muscles.
Indirect benefits of FES may include:
- Maintained or improved bone density.
- Improved heart and blood vessel function.
- Increased muscle mass.
- Decreased body fat.
- Combining FES with standard aerobic exercise like cycling may contribute to even greater benefits.
What Are the Potential Harms of FES?
- The skin under the electrodes may get irritated. You and your therapist should monitor your skin for signs of irritation or an allergic reaction.
- FES may cause autonomic dysreflexia. Immediately tell your therapist if you have signs of autonomic dysreflexia such as a pounding headache, a heart rate that is faster or slower than normal, skin redness or flushing above the injury level, cold and clammy skin below the level of injury, feeling anxious or restless, sweating, goose bumps, nasal congestion, blurred vision, and chills without fever. More information on autonomic dysreflexia is available here: https://msktc.org/sci/factsheets/autonomic-dysreflexia
- FES may cause muscle fatigue, spasms, discomfort, or soreness, especially when you start FES or increase the stimulation. Work with your therapist to make sure that the intensity and length of FES use is right for you.
- Make sure that your FES therapist is aware of issues related to SCI, like autonomic dysreflexia and skin breakdown.
How Much FES Use is Right for You?
Before you start FES, your health care provider will talk to you about how much you should use FES. They will make sure that the location of the electrodes is correct. The correct placement of the electrodes is important for reaching the target muscles. If the placement of the electrodes is not right, the stimulation will not be effective. It can also cause involuntary contractions of the muscles or undesired movements.
You should talk to your provider about these factors:
- How often you should have an FES session. Two to five times per week is typical.
- How long each FES session should be. Typical sessions last 30–60 minutes.
- The stimulation settings and the location of the electrodes.
- How intense the exercise should be.
- If your health care provider is not familiar with FES, refer them to the research-based resources listed below.
Research-Based Resources
Bekhet, A. H., Bochkezanian, V., Saab, I. M., & Gorgey, A. S. (2019). The effects of electrical stimulation parameters in managing spasticity after spinal cord injury: A systematic review. American Journal of Physical Medicine and Rehabilitation, 98(6), 484–499.
Bekhet, A. H., Jahan, A. M., Bochkezanian, V., Musselman, K. E., ElsareihHeat, A. A., & Gorgey, A. S. (2022). Effects of electrical stimulation training on body composition parameters after spinal cord injury: A systematic review. Archives of Physical Medicine and Rehabilitation, 103(6),1168–1178.
Dolbow, D. R., Gorgey, A. S., Johnston, T. E., & Bersch, I. (2023). Electrical stimulation exercise for people with spinal cord injury: A healthcare provider perspective. Journal of Clinical Medicine, 12(9), 3150. doi:10.3390/jcm12093150.
Dolbow, D. R., Gorgey, A. S., Sutor, T. W., Musselman, K., Bochkezanian, V., & Davis, G. M. (2023). Electrical stimulation exercise recommendations for individuals with spinal cord injury. Archives of Physical Medicine and Rehabilitation, 104(5), 847–851.
van der Scheer, J. W., Goosey-Tolfrey, V. L., Valentino, S. E., Davis, G. M., & Ho, C. H. (2021). Functional electrical stimulation cycling exercise after spinal cord injury: A systematic review of health and fitnessrelated outcomes. Journal of NeuroEngineering and Rehabilitation, 18(1), 99.