
Click the triangle below to listen to the podcast brief and access the transcript by clicking here.
PHASE I: Burn Evaluation & Early Care
What Is a Burn Injury?
A burn injury is damage to the layers of skin caused by exposure to the one of the below methods. Deeper burn injures may damage tissue (fat and muscle), or even bone.
- Flame: contact with fire or flames
- Flash: resulting from the heat of an explosive blast
- Scald: contact with hot liquids or hot steam
- Grease: contact with hot grease
- Contact: prolonged contact with something hot
- Electrical: electricity passing through the body and heating the skin and underlying tissue
- Chemical: contact with chemicals, such as acid or alkalis
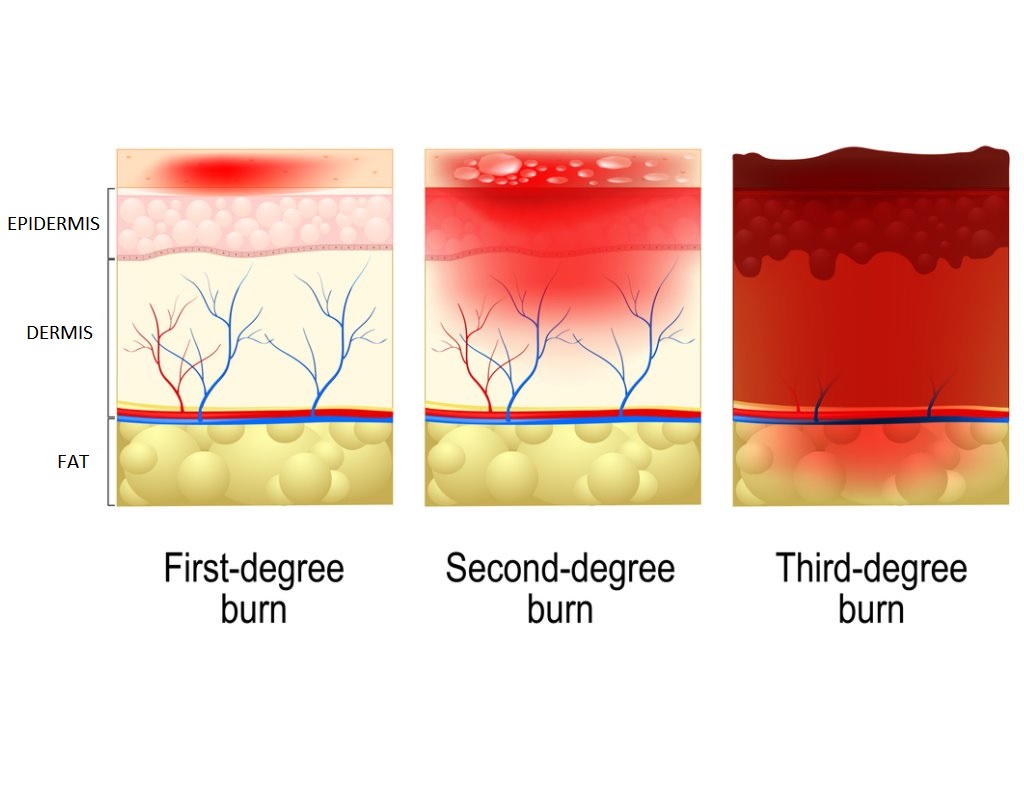
What Are the Different Degrees of Burn Injury?
Clinicians measure depth of burns in degrees:
First degree burns are the mildest type of burn. They are also called superficial burns. First degree burns damage only the epidermis, which is the first layer of skin. First degree burns usually don’t get infected or leave a scar. The skin may get red but won’t break, and they heal within 3–5 days.
Second degree burns are also called partial thickness burns. This type of burn damages the epidermis and the dermis (the second layer of skin). Second degree burns are painful. The injured area can swell and appear red with blisters. There are two subtypes of second degree burns: superficial and deep. Superficial second degree burns heal quicker (~2 weeks) and typically do not scar. Deep second degree burns take longer to heal and may require surgery depending on the size and location. They often have some degree of scarring.
Third degree burns are also called full thickness burns. This type of burn goes through the epidermis and dermis and affects deeper tissues, which may also be damaged or destroyed. The injured area can appear charred and may be black, white, or deep red in color. This area is often numb to light touch. Third degree burns don’t heal by themselves, so skin grafting is often necessary (discussed later).
Fourth degree and deeper burns destroy the skin plus fat, muscle and sometimes bone.
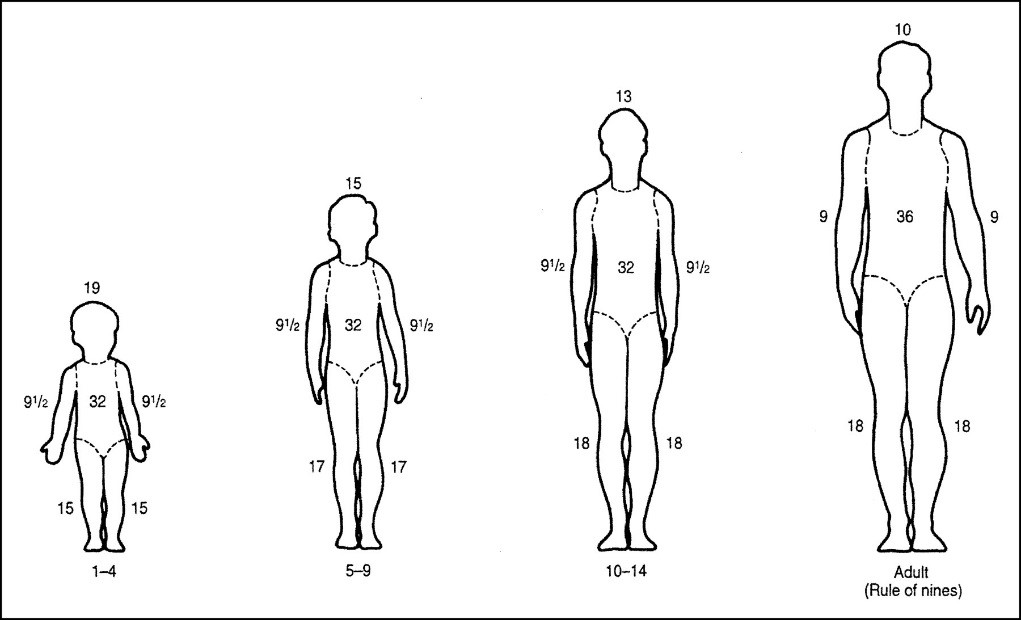
How Is the Size of the Skin Burned Estimated?
Total body surface area (or TBSA) burned is the percent (%) of the body that is burned. To estimate burn size, clinicians use a formula that considers the age of the injured person and a diagram called the Rule of Nines (shown below). This is the most common way to estimate burn size. First degree burns are not included in the calculation of percent TBSA burn.
How is the Severity of the Burn Assessed?
Clinicians consider many factors to determine the severity of a burn injury:
- Degree(depth) of the burn,
- Size (percentage) of the skin that is burned, and
- Age of the injured person
- Other factors include:
- Location of the burn on the body,
- Inhalation of toxic gases or smoke,
- Type of burn,
- Other traumatic injuries (bone fractures), and
- Other health issues (such as diabetes, heart problems, or alcoholism).
Can Lungs Be Burned?
When breathed in, smoke or toxic gases can harm the lungs. Clinicians call this an inhalation injury. This type of injury often occurs when the injured person is trapped in an enclosed area for a long amount of time. Damage depends on the type of gas and smoke particles inhaled and on length of exposure.
PHASE II: Healing the Burn
What Are Skin Grafts and Donor Sites?
Skin grafts are thin layers of skin that surgeons take from an unburned area and then surgically place on the burned area. The area where the skin is taken from is called the donor site. Common donor sites are the thigh and the back but may be taken from any uninjured area of the body other than the face. The donor site generally takes about two weeks to heal.
What Are the Different Types of Skin Grafts?
Surgeons consider many factors when deciding what type of skin graft to use. They look at the condition, thickness, and size of the wound and where the injury is on the body.
- Autograftsare permanent skin grafts that replace burned skin. With this graft, surgeons remove skin from one place on the body and place it on the burned area of the body. There are two types of autografts:
- Split-thickness skin graft involves removing the epidermis and a shallow layer of the dermis and then placing it on the burned area.
- Full-thickness skin graft involves removing the epidermis and dermis and placing it on the burned area.
- Allografts and homografts are temporary grafts to cover the wound. Donor skin comes from another person (usually a cadaver).
- Xenografts are temporary grafts to cover the wound. Donor skin comes from a pig or fish.
- Meshed grafts are grafts in which donor skin is perforated with small slits or holes. Surgeons can then expand the mesh to cover a large burned area of the body. All four types of grafts can be meshed.
- Sheet grafts are grafts that are placed on the wound directly from the donor site without being meshed. These grafts are typically used for small surface area burns and in areas where function and cosmesis (cosmetic preservation) is important.
What Should Patients Expect?
The recovery process differs for everyone. Most patients report feeling pain, fatigue, and itching during recovery and rehabilitation.
- Pain is common. Third degree burns are painful with deep pressure. Second degree burns are painful with air movement or changes in temperature. First degree burns are painful on the surface of the skin. Pain can also occur in the process of dressing changes. Most importantly, a delayed onset of increased pain can be associated with onset of wound infection. Additional information can be found in the “Managing Pain After Burn Injury” factsheet.
- Fatigue is common. The more severe the burn injury, the greater the level of fatigue.
- Itching is a common part of the healing process. Patients should never scratch their wounds. Moisturizers and antihistamines can help make the burned area less itchy. Application of cool compresses on a healed burn may also help. Additional information can be found in the “Itchy Skin After Burn Injury” factsheet.
Patients may have a tough time dealing with these symptoms, but should always let their care provider know how they feel and see what options are available to help relieve symptoms. Space is provided at the end of this factsheet for patients, family members and friends to write down questions.
What About Infection?
Burned areas can get infected, at the time of the injury and during the healing process. To prevent infection, people with burn injuries should follow the treatment orders of their health care team. They should also follow the hospital’s infection control guidelines, such as using gloves and gowns when recommended. Practicing good hand hygiene (clean hands) can help prevent infection. This applies to both the injured person and their family members, friends, and caregivers. It is also important that patients wash their wounds with mild soap and water at the time of each dressing change to decrease incidence of infection unless told otherwise. Dressings typically involve topical antibiotic ointment to prevent seeding of bacteria into the open wound bed.
What About Scarring?
Depending on the burn injury degree and location, along with age and ethnicity, scarring may occur. Unfortunately, it is difficult to predict who will develop scarring. Studies have shown that burns will typically not scar if they heal within 14 days. The longer a wound remains open, the greater the risk of scarring. Hypertrophic burn scars (raised scars in the area of the original burn) may occur and are a common complication in burn injuries. These scars may limit function depending on the location as well as affect body image. These scars may also become symptomatic and result in discomfort, itchiness, and tightness.
There are various treatments to manage hypertrophic scars including but not limited to pressure garments, silicone gel sheets, self-massage therapy and laser scar revision therapy. Consult with your provider for more information regarding these treatment modalities if you are interested.
PHASE III: Long-Term Recovery & Rehabilitation
What About Rehabilitation?
- Rehabilitation is the process of using education and therapy to help a patient reach his or her maximum potential for recovery after an injury. Rehabilitation may also include physical therapy or occupational therapy. Physical therapy treats physical impairments. It aims to improve a person’s ability to walk and move, do daily tasks, and live independently. Treatment may include exercise, splinting, bandaging, medicine, and use of assistive devices (such as crutches or walkers), massage, and joint mobilization. Below are some of the common services provided as part of rehabilitation.
- Occupational therapy uses everyday activities and materials to help patients in their own recovery. For example, a patient could practice dressing, bathing, and feeding themselves or cooking.
- Speech-language pathology helps with swallowing, voice, cognitive issues, and communication. Several types of facilities provide rehabilitation services to patients with burn injuries.
- A burn center often provides intensive physical and occupational therapy during acute hospitalization. The burn team will also follow the patient long-term, prescribing additional therapy if needed.
- An inpatient rehabilitation facility is a specially designed medical rehabilitation facility. Patients stay at the facility full-time after discharge from the burn center and must be able to do at least 3 hours of therapy per day.
- A skilled nursing facilityis a place where patients may go after they leave the burn center. Patients live in these facilities and receive medical and nursing care to help them recover.
- An outpatient rehabilitation centeris a medical facility that provides physical and occupational therapy services to people who are living at home.
What About Nutritional Needs?
Eating well is a key part of the recovery process. Healing from a burn injury requires more calories and protein than healing from other types of injury. Additional information is provided in the “Healthy Eating After Burn Injury” factsheet. Nutritionists may be available to provide information about a well-rounded diet.
What About Mental Health?
It is common to feel anxious or upset after a traumatic injury. Burns can put tremendous stress on the patient and family. Burn teams include psychologists and psychiatrists who can help with feelings and concerns. Psychiatric and psychological servicesaddress issues like depression, anxiety, post-traumatic stress, addiction, and sleep problems. Social services can help families with managing housing, finances, and navigating the healthcare system. More information can be found in the “Psychological Distress After Burn Injury” factsheet.
What Can Family and Friends Do When a Loved One is Injured and Hospitalized?
In addition to care from medical staff, patients can also draw support from family and friends. Visitors and caregivers play an important role during the recovery process. It is important for family members and friends to also take care of themselves (for example, housing, food, and care of children). It can be helpful to coordinate visiting times amongst friends and family members. Family members should also assign one person to be the main point of contact with medical staff. This person should be an adult who is available to talk with the burn team.
Other Languages
What Resources Are Available?
Factsheets s from the Burn Model System are a great source of information and discuss many topics related to burn injury, such as sleep problems, body image, social interactions, and nutrition. Factsheets are available online (http://www.msktc.org/burn/factsheets) in English and Spanish.
Videos are also available online (http://www.msktc.org/burn/videos). They cover exercise and employment after a burn injury
Feeling anxious and afraid is common after a traumatic injury. Several local and national support systems offer support and suggestions about recovering from a burn injury. Patients, family members, and friends should ask their health care team about options for support systems, such as the Phoenix Society for Burn Survivors (https://www.phoenix-society.org/). The Phoenix Society is a national peer support system in more than 60 hospitals and burn clinics throughout North America. This group is made up of burn survivors and their family members who are trained to offer support and can schedule a visit and share their recovery process.
Reference
Gauglitz, G. (2023). Hypertrophic scarring and keloids following burn injuries. In M. Jeschke & K. Collins (Eds.), UpToDate. https://www.uptodate.com/contents/hypertrophic-scarring-andkeloids-following-burn-injuries
Authorship
Understanding a Burn Injury was originally developed in 2018 by Laura C. Simko, BS, and Emily A. Ohrtman, BA, from the Boston-Harvard Burn Model System; and Gretchen J. Carrougher, MN, RN, and Nicole S. Gibran, MD, FACS, from the Northwest Regional Burn Model System, in collaboration with the Model Systems Knowledge Translation Center (MSKTC). It was reviewed and updated in 2023 by John Schulz, MD, Lauren Shepler, MPH, and Lauren Tripodi, PA, in collaboration with the MSKTC.
Source: Our health information content is based on research evidence and/or professional consensus and has been reviewed and approved by an editorial team of experts from the Burn Injury Model Systems.
Disclaimer: This information is not meant to replace the advice of a medical professional. You should consult your health care provider about specific medical concerns or treatment. The contents of this factsheet were originally developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90DP0082) and were updated under NIDILRR grants (90DPKT0009 and 90DPBU0008). NIDILRR is a Center within the Administration for Community Living (ACL), U.S. Department of Health and Human Services (HHS). The contents of this factsheet do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the federal government.
Recommended citation:Schulz, J., Shepler, L., & Tripodi, L. (2023). Understanding a burn injury [Fact sheet]. Model Systems Knowledge Translation Center (MSKTC). https://msktc.org/burn/factsheets/understanding-burninjury.
Copyright © 2023 Model Systems Knowledge Translation Center (MSKTC). May be reproduced and distributed freely with appropriate attribution. Prior permission must be obtained for inclusion in fee-based materials.