
Consciousness is an awareness of one’s self and surroundings. Brain injury can cause disorders of consciousness (DOC). Some injuries are mild; they may cause minor changes in consciousness such as brief confusion. Severe injuries can cause permanent unconsciousness.
Of people with severe injuries, 60% to 80% survive. Many of those who survive are completely unconscious for some period. During this time, they aren’t aware of themselves or the world around them. A state of complete unconsciousness with no eye-opening is called coma. A state of complete unconsciousness with some eye-opening and periods of wakefulness and sleep is called the vegetative state (VS). This refers to the “vegetative functions” of the brain (regulating body temperature, breathing, etc.) which often return before return of consciousness. (The VS is also called unresponsive wakefulness syndrome.) As people recover from severe brain injury, they usually go through several phases of recovery. Recovery through these phases can slow or stop.
- Coma
- Vegetative State
- Minimally Conscious State
- Confusional State
- Full Consciousness (often with specific impairments)
Features of coma
- No eye-opening
- Unable to follow instructions
- No speech or other forms of communication
- No purposeful movement
Features of VS
- Return of a sleep-wake cycle with periods of eye opening and eye closing
- May moan or make other sounds especially when tight muscles are stretched
- May cry or smile or make other facial expressions without apparent cause
- May briefly move eyes toward persons or objects
- May react to a loud sound with a startle
- Can’t follow instructions.
- No speech or other forms of communication
- No purposeful movement
Care during coma or VS
People in a coma or a VS need a lot of care. This care may include:
- Feeding with a feeding tube.
- Turning the person while he or she is in bed to prevent pressure injuries (“pressure sores”).
- Helping with bowel and bladder relief. This may include using a catheter or diapers.
- Managing breathing. This may include removing mucus from the airway. It may also include cleaning a tracheostomy tube.
- Managing muscle tone. This includes helping to relieve extremely tight muscles with positioning and range of motion exercises.
- Using special equipment. This may include a wheelchair. It could also include special bedding to help with proper posture, decrease muscle tightness, and prevent pressure sores.
- Treating infections such as pneumonia or urinary tract infections.
- Managing other health problems such as fevers or seizures.
What happens after coma and the VS?
The first sign of consciousness is usually visual tracking. This occurs when the patient’s eyes follow people or an object. Other signs include:
- Following simple instructions such as, “Squeeze my hand,” or “Say your name.”
- Communicating by saying words or indicating yes or no with head nods or gestures.
- Engaging in “automatic” behaviors like scratching the skin or crossing/uncrossing the legs.
People with brain injury will recover consciousness at a slow or fast rate, based on how severe their injury is. For people with very severe injuries, return of consciousness is a slow process. People with less severe injuries may move through the phases listed above quickly. Some of the stages described here may not be recognized or may not occur at all. For people with very severe injuries, recovery may stop at one of these stages.
Coma rarely lasts more than 4 weeks. Some patients move from coma to the VS. Others may move from coma to partial consciousness. It is rare for a person with severe brain injury to move directly from coma, or the VS, to full consciousness. People who are unconscious for a short time generally have had a less severe brain injury. As a result, they are likely to have a better recovery than people who are unconscious for a long time.
Of people who are in the VS 1 month after traumatic brain injury (TBI – when brain damage is caused by a physical impact such as a car crash or fall), 60% to 90% will regain consciousness by 1 year after injury. They will likely have a slow recovery. They usually have ongoing cognitive and physical difficulties. People who are in the VS due to stroke, loss of oxygen to the brain (anoxia), or some types of severe illness may not recover as well as those with TBI. People who remain in a prolonged VS may live for a long time. But they often have complications such as pneumonia, respiratory failure, or infections, which may shorten their life expectancy.
Another stage of recovery is called the minimally conscious state, or MCS. People in the MCS can’t respond or communicate consistently.
Features of MCS
- May follow simple instructions.
- May indicate yes or no by talking or gesturing.
- May speak some words or phrases that others can understand.
- May make automatic movements. These may include scratching their head, crossing their legs, or moving their hair out of their eyes.
- May respond to people, things, or other events by:
- Crying, smiling, or laughing;
- Making sounds or gesturing;
- Reaching for objects;
- Trying to hold or use an object or
- Keeping the eyes focused on people or things for a sustained period of time whether they are moving or staying still.
People in the MCS can do one or more of these things, but not consistently. For example, a person may follow a simple instruction one time; another time, they may not follow any instructions at all. This may make it hard to know if a person is in the VS or the MCS. People in the MCS need a lot of care just like people in the VS.
Recovering from the MCS
When a person can correctly answer simple “yes” and “no” questions or use at least two objects such as a comb or pencil consistently, they are no longer in the MCS. Some people stay in the MCS indefinitely, but many improve and regain independence. The longer a person remains in the MCS, the more permanent impairments he or she is likely to have. Both the VS and the MCS are caused by severe damage to areas of the brain that are important for consciousness. After improving from the MCS, people are usually confused. Some people move directly from coma to this confused state.
Features of the confusional state
- Acting lost or confused. This may include not being able to keep track of the correct place and time.
- Severe problems with attention, memory, and other mental abilities.
- Changes in level of responsiveness.
- Restlessness.
- Disrupted nighttime sleep.
- Feeling very tired and sleeping during the day.
- Believing things that aren’t true.
- Seeing things that aren’t there.
Comparison of Coma, Vegetative State, and Minimally Conscious State
|
|
Coma |
Vegetative State |
Minimally Conscious State |
|
Eye Opening |
No |
Yes |
Yes |
|
Sleep/Wake Cycles |
No |
Yes |
Yes |
|
Visual Tracking |
No |
No |
Often |
|
Object Recognition |
No |
No |
Inconsistent |
|
Command Following |
No |
No |
Inconsistent |
|
Communication |
No |
No |
Inconsistent |
|
Contingent Emotion |
No |
No |
Inconsistent |
As with the VS and MCS, how fast people recover and how much they recover from the confusional state may vary. Most people who reach the confusional state make further progress. The severity of their brain injury and related health problems determine the degree of recovery. The less time the person is in the confusional state, the better their recovery will be. Mild problems such as poor sleep or urinary tract infections may lengthen the confusional state, but they may not affect the outcome.
Once the confusional state ends, people can usually pay attention, keep track of place and time, and hold onto memories of daily experiences again. They will likely still have serious cognitive problems such as impaired attention or memory or slowed thinking. These problems are likely to get better over time. While some people make limited progress, others make a good deal of progress.
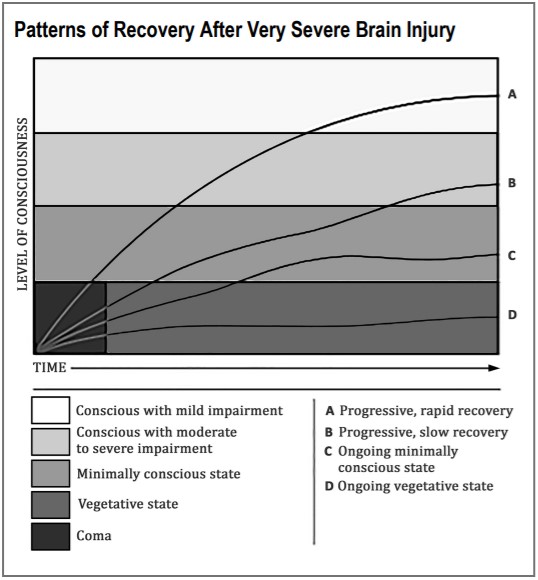
This image shows patterns of recovery that may follow coma. Some people wake up quickly from coma; they may briefly stay in the MCS before further recovery. They may also have mild impairments. Others may be in the MCS for a long time after emerging from the VS. They usually have more long-term impairment. Slow recovery may continue for several years, especially for those with traumatic injuries. Sometimes, people stay in the VS or MCS for a long time. In some cases, these conditions may be permanent.
What treatments are used with people in the VS or MCS?
Only one treatment has been shown to help patients with TBI regain consciousness faster. Amantadine is a drug previously used in Parkinson’s disease. When started between 4 and 16 weeks after TBI, it increases the speed of recovery. But it’s not known whether it changes the long-term outcome or only reduces the time to reach that outcome. Its effect on patients with nontraumatic injuries (damage to the brain from medical causes) is not known.
How often health care facilities and doctors use treatments such as medicines or sensory stimulation (stimulating the person with sights, sounds, touches, etc.) to help patients regain consciousness varies. Because the degree of recovery from DOC varies, it’s hard to judge the value of these and other treatments outside of research studies. You can talk to your loved one’s doctor about using these treatments. Many patients may have good recoveries with good medical and rehabilitative care. Unproven treatments may slow recovery or have other bad effects or no effect; they may also improve recovery
Transitions to different levels of care
During recovery, people in the VS or the MCS may get care in many settings. A person with a DOC will likely start treatment in an acute care hospital; the focus is on saving the patient’s life and stabilizing the patient. Once those needs are met, the focus moves to restoring as much function as possible. Sometimes this takes place in an acute rehabilitation hospital. These hospitals provide high-intensity, team-oriented services. Services include physical therapy, occupational therapy, speech-language therapy, recreational therapy, neuropsychological services, and medical and nursing care.
Some patients don’t go from the acute care hospital to an acute rehab program. These patients may go directly to a long-term acute care hospital (LTACH or “L-tack”), a skilled nursing facility (SNF or “sniff”), a subacute (less intensive) rehab program, or a nursing home. They may also go home with family or have home health care or outpatient treatment. People who get care in an acute rehab program first are usually discharged to one of these places as well.
The quantity and quality of medical management, nursing care, and rehab services offered in SNFs, subacute rehab programs, and nursing homes varies. Experts recommend that patients with DOC be discharged from acute care to an acute inpatient rehab program. These programs are more likely to provide the medical and rehab expertise needed. Also, they offer the team-oriented treatment planning that such patients need soon after injury. But many insurers still encourage patients to get treatment in less intensive settings that don’t specialize in severe brain injury. Your loved one’s doctor may be able to speak with your insurance company about the importance of receiving care in inpatient rehabilitation. Most insurance companies also have an appeal process that may include additional review of the admission request.
When patients are medically unstable or don’t show signs of recovery for a long time, doctors may consider palliative care. In this type of care, the focus of treatment shifts from recovery to comfort.
Many factors affect where a person with severe DOC or other severe impairments goes after leaving an acute care hospital or rehab program. These factors include:
- The person’s medical condition.
- Health insurance coverage and other benefits.
- The person’s ability to benefit from rehab therapies such as physical, occupational, and speech-language therapy.
- The doctor’s recommendation about where people should go to continue to recover after severe injuries.
- The family’s ability to care for the person at home.
- The family’s wishes.
- Practical matters such as the distance the family has to travel to visit the person at the facility.
The names used to describe levels of care and the settings in which care is given vary across the country. It’s helpful to work with a social worker or case manager in the facility where your loved one is getting care to plan any needed moves. Don’t be afraid to ask questions to make sure that you get the information you need to help make the best decision.
Things to look for when considering a setting to care for your loved one:
Here are some things to look for when choosing a place for care:
- Your family member’s current treatment team has received good feedback about the program’s quality of care when they have referred others there.
- The staff make you feel comfortable. They are available to talk about your concerns, and they answer your questions.
- The program has a multidisciplinary treatment team that, at a minimum, includes a rehabilitation physician, nurse, speech pathologist, physical therapist, occupational therapist, psychologist, and social worker.
- The treatment team meets together to identify treatment goals and review progress.
- The program and treatment staff have worked with the same kinds of problems that your family member has.
- The facility knows about the specific care your loved one needs and can meet those needs. You can help to make sure that a detailed nursing care plan is created.
- The program includes case management to help plan for the next level of care, whether it’s moving to a rehabilitation program, an LTACH, a SNF, or home.
- The program provides education and training for future caregivers.
- The program has a systematic approach to measure progress in all patients.
- The program is guided by recommendations for rehab programs from the American Congress of Rehabilitation Medicine and the NIDILRR’s Traumatic Brain Injury Model System.
- The program receives good grades in state and/or federal quality ratings
If support services can be arranged, some persons in the VS or the MCS can be cared for at home.
Thoughts from families who have been there
Family members who have had a loved one in the VS or the MCS have identified a few important issues to keep in mind.
1. Communicating with healthcare providers
Be sure to ask questions, share your observations, and express your opinions.
2. Managing medical equipment and supplies
It’s important to know about your loved one’s equipment and supplies. You should also know how to communicate with the companies who provide these items.
3. Providing care
Family members often provide some care for their loved ones. In some cases, they may get paid for doing so. The amount of care you provide will depend on.
- Your role. This can range from providing most of the care yourself to directing the care provided by others.
- The people who help you provide care. These may include sitters, attendants, nurses, and family members.
- The setting. This could be your home or a skilled nursing facility.
- The guidance you get from health care providers. It’s best to get as much training as possible on the types of care you choose to provide and can manage. Such care may include bathing and grooming, bowel and bladder management, mobility and range of motion exercises, and management of other health problems that your loved one may have.
4. Learning about financial resources
You may feel overwhelmed as you learn about the financial resources that may or may not be available to your loved one. But with patience, persistence, and help from others, you will figure out which programs apply and find your way through the application processes.
Some programs that you will want to learn about include:
- Health care programs such as Medicare and Medicaid.
- Income replacement or financial assistance programs such as Social Security Disability Insurance (SSDI) or Supplemental Security Income (SSI). You may also want to find out if your loved one had disability insurance through work.
- Services to help with community living such as state and community agencies that assist people in these areas. For instance, some states have Medicaid waiver programs that provide funding for in-home care to allow people to stay at home.
You may not find someone who knows all there is to know about how to access these services and programs. The key is to ask questions and follow up to make sure that you and your loved one get all the benefits available. Social workers, therapists, case managers, and your local social security office may be helpful. Others who may be able to help include your state brain injury association chapter, family members or friends who are disabled or who have family who are disabled, or the human resources department at your loved one’s work.
5. Guardianship
If your loved one named a health care proxy before the injury, that person will be able to make health care decisions on your loved one’s behalf. Because your loved one may not be able to make decisions for himself or herself for a while, it may be helpful for you, or someone else, to be named as guardian. A guardian has the legal authority to make medical and/or financial decisions for someone who lacks the ability to do so. This may make it easier to handle medical decisions or manage your loved one’s financial matters. If you think that your loved one may need a guardian, you will need to contact an attorney for help. Guardianship can be reversed when it is no longer needed.
How to interact with a loved one who is unconscious or at a low level of responsiveness
The most natural way of interacting is to talk to your loved one, even though he or she may not respond or understand. Telling him or her about recent events in your life, what’s going on in your family or neighborhood, or the latest news may make you feel connected. Talking with your loved one about what you are doing as you provide care can increase your comfort with caregiving. For example, telling your loved one that you are going to move his or her arms and legs to help prevent joint tightness might make you feel more comfortable with this task. Only do these range of motion exercises if you have been instructed to do so by a doctor, nurse, or therapist.
Touch is another way to feel connected. Some family members have said that giving a massage or putting lotion on the hands or face of their loved one helps them to feel close to them. It’s also important to give your loved one time for quiet and rest, such as by turning the TV off. You should also avoid overstimulation as this may cause rapid breathing, muscle tightening, teeth grinding, restlessness, and fatigue.
Taking care of yourself and other family members
Family members of a person in the VS or the MCS often feel a sense of loss or grief for the relationship they had before the injury. You can cope with these feelings in a few ways. A person in the VS or the MCS may make slow progress or go for long periods with no progress. Keeping a journal of the changes you have seen may be comforting. This may let you see how your loved one is more able to respond than he or she was at an earlier point in time.
Having a loved one who is in the VS or the MCS can be physically and emotionally draining. Dealing with this alone can be too much for one person. It’s important to rely on support from others. You can look to existing supports, such as family, friends, and religious groups. You can also find new supports.
Other resources to consider include support groups and agencies, and the internet. You can contact the Brain Injury Association of America’s (BIAA) National Brain Injury Information Center (www.biausa.org, 1-800-444-6443). The BIAA can give you contact information for the closest chapter of your state brain injury association. Health care providers such as doctors, therapists, and social workers may also be good sources of information about supports available to you
Even the most committed caregivers need time for themselves. If your loved one is still in the hospital or living in a nursing care facility, you could create a rotating visitation schedule. This will give you a break while giving other friends and family a chance to spend time with your loved one. If your loved one is at home, you could ask a friend or family member to give you a 2-hour break to go do something for yourself. You could also hire full-time caregivers for a week or have your loved one spend time in a nursing care facility or hospital.
When your loved one was first injured, you were likely in crisis mode, focusing on problems and putting the rest of life on hold. As time goes by, you will need to shift from crisis mode to dealing with everyday matters such as paying bills, maintaining relationships with other family members, and taking care of your own physical and mental health. Although it’s normal to want to focus on your injured loved one, other family members have needs. For some people, getting counseling from a therapist or clergy member can help them to adjust to the life changes that have occurred due to their loved one’s injury.
Caring for a person in the VS or the MCS is a big challenge. But using appropriate resources, as described in this factsheet, can be a big help. Each person will respond differently to this challenge. But almost everyone can cope and move forward. Many family members feel a deep sense of personal satisfaction in making life comfortable and pleasant for a loved one with a severe injury.
Reference
1 Giacino, J. T., Katz, D. I., Schiff, N. D., Whyte, J., Ashman, E., Ashwal, S., Barbano, R. L., Hammond, F., Laureys, S., Ling, G. S. F., Nakase-Richardson, R., Seel, R. T., Yablon, S. A., Getchius, T. G., Gronseth, G., & Armstrong, M. J. (2018). Practice guideline recommendations summary: Disorders of consciousness. Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology; the American Congress of Rehabilitation Medicine; and the National Institute on Disability, Independent Living and Rehabilitation Research. Neurology, 91(10), 450–460. DOI:10.1212/WNL.0000000000005926. This article was published simultaneously in Archives of Physical Medicine and Rehabilitation (Giacino et al., 2018, Archives of Physical Medicine and Rehabilitation, 99(9),1699–1709).
Sherer M, Vaccaro M, Whyte J, Giacino JT, & the Consciousness Consortium. Facts about the Vegetative and Minimally Conscious States after Severe Brain Injury 2007. Houston: The Consciousness Consortium.
Authorship
Facts About the Vegetative and Minimally Conscious States After Severe Brain Injury was developed by Sherer M, Vaccaro M, Whyte J, Giacino JT, Childs N, Eifert B, Katz, DI, Long DF, Novak P, Cho S, & Yablon SA and the Consciousness Consortium in 2007.
Factsheet Update
Facts About the Vegetative and Minimally Conscious States After Severe Brain Injury was reviewed and updated by John Whyte, MD, David Glazer, MD, Thomas Watanabe, MD, Joseph Giacino, PhD, and Amy Rosenbaum, PhD, in collaboration with the American Institutes for Research Model Systems Knowledge Translation Center.
Source: The content in this factsheet is based on research and/or professional consensus. This content has been reviewed and approved by experts from the Traumatic Brain Injury Model Systems (TBIMS), funded by the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR), as well as experts from the Polytrauma Rehabilitation Centers (PRCs), with funding from the U.S. Department of Veterans Affairs.
Disclaimer: This information is not meant to replace the advice of a medical professional. You should consult your health care provider regarding specific medical concerns or treatment. This publication was produced with funding from the National Institute on Disability, and Rehabilitation Research in the U.S. Department of Education, grant no. H133A031713. It was updated by the TBI Model Systems in collaboration with the American Institutes for Research Model Systems Knowledge Translation Center, with funding from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90DP0082). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this factsheet do not necessarily represent the policy of NIDILRR, ACL, or HHS, and you should not assume endorsement by the federal government.
Copyright © 2020 Model Systems Knowledge Translation Center (MSKTC). May be reproduced and distributed freely with appropriate attribution. Prior permission must be obtained for inclusion in fee-based materials