
What is a pressure injury?
Pressure injury is a newer term for what people might know as a pressure sore, pressure ulcer, decubitus ulcer, bedsore or skin breakdown. The term changed because not all stages of injuries caused by pressure are actually open “sores” or “ulcers.” However, the meaning is similar. A pressure injury is an area of the skin or underlying tissue (muscle, bone) that is damaged when prolonged pressure cuts off blood flow to the area for too long.
- To learn more about skin care, visit https://msktc.org/sci/factsheets/skincare.
What Is Surgical and Reconstructive Treatment?
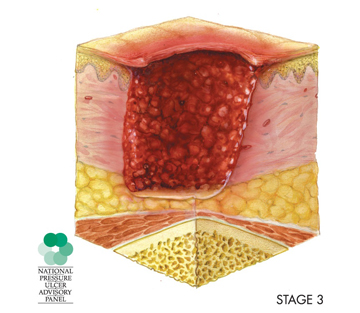
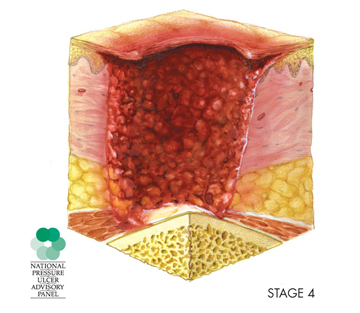
Stage 3 and 4 pressure injuries are wounds that most often need surgical and reconstructive treatment to promote healing.
- Stage 3 is a wound that extends from the first layer of the skin (epidermis), through the second layer (dermis), and into the fatty tissue below (subcutaneous tissue).
- Stage 4 is a wound that extends past the fatty tissue and into the muscle tissue. It can also extend to the bone.
Surgical Treatment
During surgery, the wound is cleaned (debrided) to remove any dead or infected tissue, which sometimes includes removing some bone. This process creates a larger wound, but the remaining tissue is healthy and more likely to heal.
Reconstructive Treatment
Reconstructive treatment is most often done in one of two ways using a section of healthy skin and tissue known as a “flap.”
- A flap of healthy skin and tissue near the wound is partly detached and pulled over the wound. This allows part of the flap to stay attached to the blood vessels connected to healthy skin and tissue. That blood supply helps nourish the skin and tissue pulled over the wound.
- A flap of healthy skin and tissue is completely detached (sometimes called harvested) from the back, buttocks, or thigh and moved to cover the wound.
- There are rare times when amputating a leg may need to be considered if a lot of skin and tissue needs to be taken from the leg to cover a large wound elsewhere on the body.
Where on the Body Is the Treatment Usually Needed?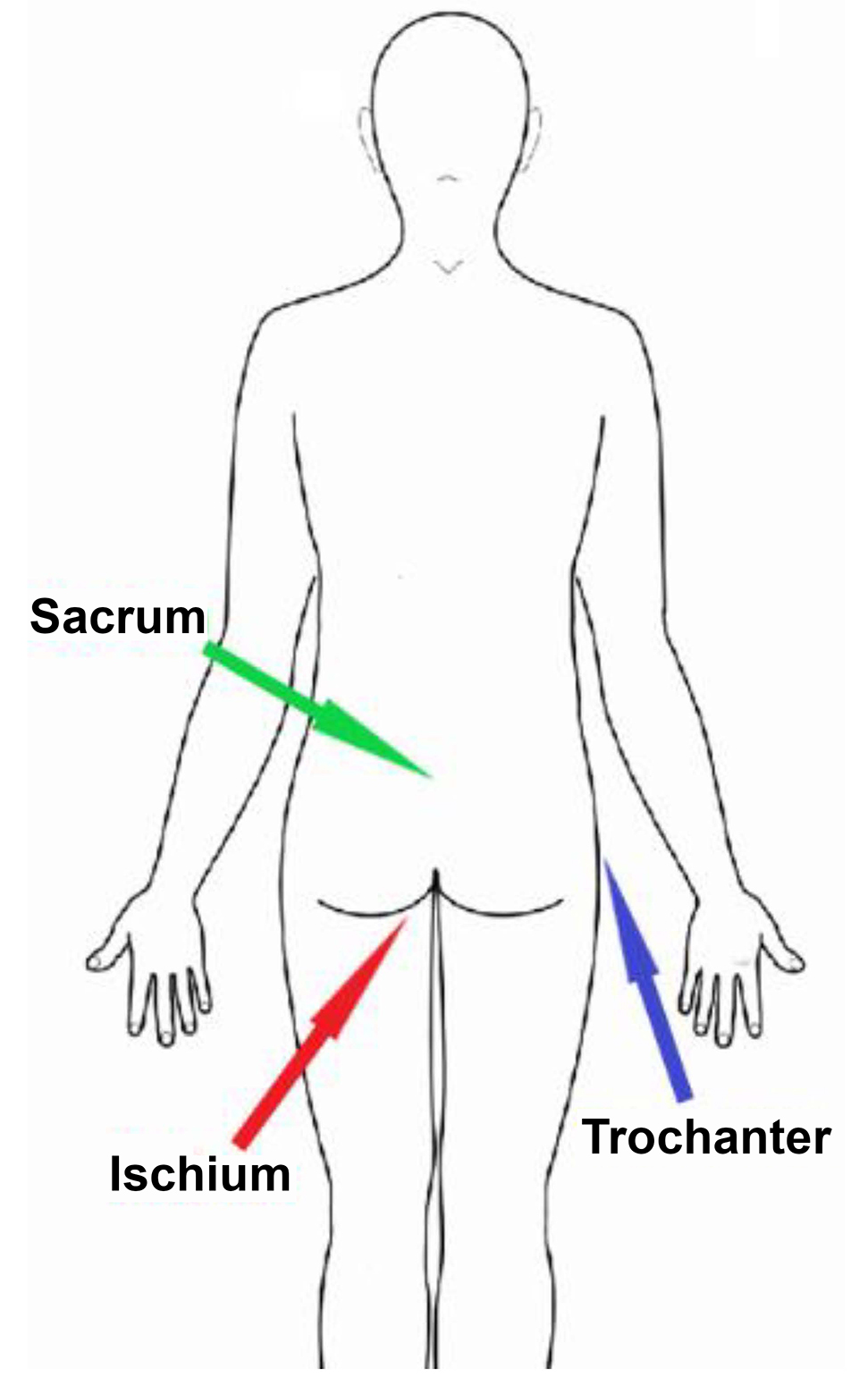
- Ischium (pronounced ish·e·um) – This is the bony area above the back side of the thigh and beneath the buttocks. A pressure injury can develop here when you sit too long without shifting your weight.
- Sacrum (pronounced sac·rum) – This is the bone in the center of your lower back just above your buttocks. A pressure injury can develop here when you lie on your back too long without turning or stay in a reclined position too long without sitting up.
- Trochanter (pronounced tro·can·ter) – This is the boney area on the side of your hip. A pressure injury can develop here when you lie on your side too long without turning.
What Are the Benefits of This Treatment?
It can take several months of bedrest for a severe wound to heal on its own. All pressure must be off the area while in bed, which can be very hard to do on an ongoing basis. If pressure is put on the area while in bed, it can delay healing or make the wound worse. Plus, there is an increased risk of infection with any open wound. The longer the wound is open, the longer the higher risk continues. If an infection develops, there is a risk that it can spread and become life-threatening.
The obvious benefit of this treatment is that the wound can heal much quicker than it would without the treatment. Your doctor can explain all your benefits, but here are a few of the benefits:
- Much less time needed for bedrest
- Lowered risk for infection
- Improved quality of life
- Increased independence to enjoy meaningful activities
- Lowered healthcare costs
What Are the Risks of this Treatment?
Problems can happen during any surgery, even with the best treatment. Your surgeon will talk with you to explain what problems might happen. It is up to you to decide whether the benefits of the surgery outweigh the possible risk for problems. Here are a few examples of the more potential serious problems you will talk about with your doctor:
- The wound comes back
- The wound either does not close properly or breaks open along the row of stitches holding the flap edges together
- Harmful bacteria get into the body through an opening in the skin and leads to an infection
- The skin and tissue used for the flap dies
- Bleeding occurs under the flap that may need emergency treatment to drain
Am I a Good Candidate for This Treatment?
Each person is different, and each injury is different. So talk to your medical team to find out if this treatment is a good option for you. In general, it is important to talk about some of the key factors that can give you the best chance for wound healing after surgery. Here are a few of the factors you will talk about with your doctor:
- Your support system – you are responsible for your own health, but your best chance for success is if you have good support from people who are close to you.
- Proper equipment – using proper equipment is critical to promote healing after treatment, effective long-term care, and prevention of potential setbacks.
- Healthy diet – water, folic acid, iron, zinc, and Vitamins B6, B12, and C are a few key parts of a healthy diet that are helpful in skin care and wound healing. It is best to talk with a dietitian to work out a diet that suits your personal needs and tastes.
- Managing health conditions – a primary care doctor or specialist is needed to manage medical concerns like blood pressure, diabetes, incontinence, and other conditions you have.
- Tobacco and nicotine products – skin is damaged and wound healing is hindered by products like cigarettes, cigars, smokeless tobacco, or any electronic nicotine delivery system like e-cigarettes and e-vaporizers.
- Alcohol or drug use – use damages skin and hinders wound healing.
What Can I Do to Give My Wound the Best Chance to Heal?
You should always follow the advice of your medical team to have the best outcomes. It is also important to prepare as best as you can for what is ahead.
Preparing Yourself
You have to prepare yourself mentally to be ready for recovery. It can take weeks to recover from surgical and reconstructive treatment. This means prolonged bedrest and time to rebuild strength and stamina once you begin the transition from bedrest to sitting up again. It also means your social life will be limited during that time.
- It is human nature to rush through recovery, but you can help prevent setbacks by being patient with the healing process. It might be helpful to think of recovery as a short-term sacrifice for a long-term gain.
- You can plan ahead to find ways that you can fill your time and engage your mind. You might play video games, enjoy a book (hard-copy or audio book), listen to music or podcasts, or binge watch movies and TV.
- You may also need to make some personal changes to give yourself the chances for recovery. For example, you may need to change your diet, manage health conditions, and stop using any tobacco and nicotine product.
- Tobacco and nicotine products are especially bad because using them narrows the blood vessels to your skin. This means that your skin cannot get as much oxygen and nutrients because of impaired blood flow, so the wound and the flap will not heal properly.
Preparing for Surgery
You and your surgeon will discuss ways to help avoid problems that can happen during the surgery. Here are some common topics you will likely discuss before surgery:
- A wound care history is needed to know how long the wound has been present, if there are other wounds, and what treatments have been done already.
- A health evaluation is needed to get blood work, x-rays, and a review of your diet and current secondary medical conditions.
- Muscle spasms (spasticity) are a common after SCI. They must be well controlled to keep spasm movements from damaging the flap.
- Any current infection is treated.
- A medical test may be done to check for a urinary tract infection.
- Redness at the wound edge, a foul odor, and pus are signs of an infection.
Preparing to Go Home After Surgery
Your discharge recovery plan will be made before surgery. Your care plan will focus on doing everything possible to promote healing and prevent problems.
- You will need to be taught wound care, or your family will need to be taught if they are going to help manage your care. Normally, not much wound care is needed other than cleaning, keeping the area dry, and managing any wound drains.
- Home health care or a stay in a skilled nursing facility may be set up if needed.
- Follow-ups with your doctor as needed.
- You must have the proper equipment to promote healing and help prevent future skin problems.
- A pressure-reducing mattress (such as a low air loss mattress or an air fluidized bed). You will lie on this air or fluid bed to reduce pressure on the healing wound.
- A pressure-reducing seat cushion. Pressure mapping should be done for wheelchair users to ensure that the best cushion is used. Pressure mapping uses a thin, sensor mat on the wheelchair seat. A computer screen displays how well your weight is spread across the seat surface. Spreading weight out help reduce pressure points that are more likely to damage the skin.
- Continue to do regular pressure reliefs (sometimes called weight shifting, pressure redistribution, and pressure reduction) exactly as recommended by your treatment team. You need to take great care when doing pressure reliefs to avoid bumping, shearing, and other stresses to the wound.
- It is vital that you give the area time to heal before putting pressure back on it. You can easily re-injure the area if you put pressure on it too soon.
- Sitting protocol – You will slowly begin the transition from bed rest to sitting in your wheelchair once the wound has had time to heal. It’s common to sit for short lengths of time, maybe 15 minutes, for only a few times per day at first. The time you spend sitting will gradually increase as the wound continues to heal.
What If I Have More Than One Pressure Injury?
You and your surgeon will decide whether more than one surgery is needed if you have more than one severe wound.
What Do I Do If I Have Questions?
- Ask your doctor to explain anything you do not understand.
- This treatment cannot restore normal sensation in areas that have lost sensation because of the SCI.
- Ask for information that explains in detail all the possible risks and benefits of the treatment.
- You can learn more by reading the factsheet, “Skin Care and Pressure Sores in Spinal Cord Injury” at https://msktc.org/sci/factsheets/skincare.
References
Terminology on pressure injuries and stages of pressure injuries is based on education and clinical resources provided by the National Pressure Ulcer Advisory Panel (http://www.npuap.org). The panel serves as the authoritative voice for improved patient outcomes in pressure injury prevention and treatment through public policy, education, and research.
Authorship
Surgical and Reconstructive Treatment of Pressure Injuries was developed by Jorge de la Torre, M.D., F.A.C.S., M.S.H.A.; Cheryl Lane, DNP, ANP & FNP, CWCN, CRRN; and Phil Klebine, M.A in collaboration with the Model Systems Knowledge Translation Center.
Source: The content in this factsheet is based on research evidence and/or professional consensus and has been reviewed and approved by an editorial team of experts from the Spinal Cord Injury Model Systems (SCIMS), funded by the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR).
Disclaimer: This information is not meant to replace the advice of a medical professional. You should consult your health care provider regarding specific medical concerns or treatment. The contents of this factsheet were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90DP0082). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents of this factsheet do not necessarily represent the policy of NIDILRR, ACL, HHS, and you should not assume endorsement by the Federal Government.
Copyright © 2019 Model Systems Knowledge Translation Center (MSKTC). May be reproduced and distributed freely with appropriate attribution. Prior permission must be obtained for inclusion in fee-based materials.